Drug resistance in malaria infection
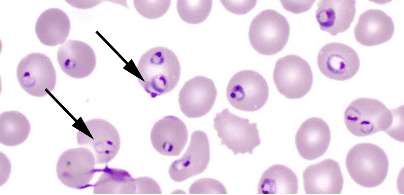
The malaria parasite, Plasmodium falciparum, has developed resistance to most of the available antimalarial drugs currently in use. Recent report indicates that, elsewhere, the parasites have developed resistance even to the newly introduced artemisinin-based combination therapy (ACT). Going forward, it is important to attempt to understand the mechanisms of resistance to the antimalarial drugs and then identify new drug targets as well as discover novel anti-plasmodia compounds. Concurrently, there is the need to monitor the efficacy of the ACT which are currently in use in most disease endemic areas. Our group is engaged in multiple studies purposely to address some of these issues including identifying the factors and variation in the parasite that affect its susceptibility to antimalarial drugs. These are being pursued through:
- Interrogation of the unique metabolic pathways (eg. Purine transport system) of the parasite in order to identify novel antimalarial drug targets.
- Using CRISPR Cas 9 gene editing techniques to identify molecular markers of antimalarial drug resistance and drug target discovery.
- Monitoring resistance to antimalarial drugs using WHO recommended standardized methods.
Our research has led to the discovery of novel purine transport pathways in Plasmodium falciparum. We have also generated data from field activities on the efficacy of antimalarial drugs in Ghana. Previously, we introduced the use of SYBR Green method in Ghana which offered a cheap and reliable means of evaluating the outcome of in vitro drug test. Together with external collaborators, we developed the ‘In Vitro Analysis and Reporting Tool (IVART)’ which removes the subjectivity from in vitro malaria drug sensitivity assay analysis among others.
- Abuaku B, Duah-Quashie NO, Quashie N, Gyasi A, Afriyie PO, Owusu-Antwi F, Ghansah A, Malm KL, Bart-Plange C, Koram KA (2021).Trends and predictive factors for treatment failure following artemisinin-based combination therapy among children with uncomplicated malaria in Ghana: 2005-2018. BMC Infect Dis. 21(1):1255.
- Ofir-Birin Y, Ben Ami Pilo H, Cruz Camacho A, Rudik A, Rivkin A, Revach OY, Nir N, Block Tamin T, Abou Karam P, Kiper E, Peleg Y, Nevo R, Solomon A, Havkin-Solomon T, Rojas A, Rotkopf R, Porat Z, Avni D, Schwartz E, Zillinger T, Hartmann G, Di Pizio A, Quashie NB, et al., (2021). Malaria parasites both repress host CXCL10 and use it as a cue for growth acceleration . Nat Commun. 12(1):4851.
- Tandoh KZ, Wilson MD, Quashie NB, Duah-Quashie NO (2021).Implicating extracellular vesicles in Plasmodium falciparum artemisinin resistance development.Traffic 22(6):194-200.
- Abuaku B, Duah N, Quaye L, Quashie N, Malm K, Bart-Plange C, Koram K (2016).Therapeutic efficacy of artesunate-amodiaquine and artemether-lumefantrine combinations in the treatment of uncomplicated malaria in two ecological zones in Ghana. Malar J. 15(1):6.
- Quashie NB, Duah NO., Abuaku B, Quaye L, Ayanful R, Akwoviah GA, Kweku M, Duplessis C, Johnson J, Lucchi NW, Udhayakumar V, Kronmann KC, Koram KA (2013). A SYBR Green-based in vitro test of susceptibility of Ghanaian Plasmodium falciparum clinical isolates to a panel of antimalarial drugs. Malar J. 12:450
- Woodrow CJ, Dahlström S, Cooksey R, Flegg JA, Le Nagard H, Mentré F, Murillo C, Ménard D, Nosten F, Sriprawat K, Musset L, Quashie NB, Lim P, Fairhurst RM, Nsobya SL, Sinou V, Noedl H, Pradines B, Johnson JD, Guerin PJ, Sibley CH, Le Bras (2013). High-throughput analysis of antimalarialal susceptibility data by the WorldWide Antimalarial Resistance Network (WWARN) in vitro analysis and reporting tool. J.Antimicrob Agents Chemother.57 (7):3121-30
- Quashie NB, Ranford-Cartwright LC and de Koning HP (2010). Uptake of purines in Plasmodium falciparum-infected human erythrocytes is mostly mediated by the human Equilibrative Nucleoside Transporter hENT1 and the human Facilitative Nucleobase Transporter hFNT1. Malar J. 9:36
- Quashie NB, Dorin-Semblat D, Bray PG, Doerig C, Ranford-Cartwright LC and de Koning HP (2008).A comprehensive model of purine uptake by the malaria parasite Plasmodium falciparum: identification of four purine transport activities in intraerythrocytic parasites. Biochem J. Apr 15; 411(2):287-95
- Quashie NB, Duah N, Abuaku B, Koram KA (2007). The in-vitro susceptibilities of Ghanaian Plasmodium falciparum to antimalarial drugs. Ann Trop Med Parasitol. 101(5):391-8